Pulmonary Anatomy and Physiology
Pulmonary Anatomy and Physiology
The major purpose of breathing is to supply O2 and to remove CO2 from cells
Four major functions to achieve this goal:
1. Pulmonary ventilation: movement of air into and out of lungs
2. Diffusion of O2 and CO2 between the alveoli and the blood
3. Transport of O2 and CO2 in the blood to and from cells
4. Control of ventilation
Once the O2 is transferred to the cells it is utilized to metabolize various food molecules involving a series of enzymatic reactions. During this process there is release of energy which is stored in the form of ATP-This process is called cellular respiration.
From the time of birth until our death we breath continuously at a rate of 12-15 breaths/min. However, breathing can change in response to alterations in blood chemistry.
Breathing and gas exchange can increase 20-fold to meet the body’s energy demands during periods of need such as exercise.
I. BASIC ANATOMY:.
The lungs are composed of 2 treelike structures:
1. Vascular tree: consists of arteries and veins connected by capillaries
2. Airway tree: consists of hollow branching tubes that conduct air from the environment to site of gas exchange to the blood.
Conducting Zone: (in descending order): Nose (conchae)-Pharynx-Larynx-Trachea-Bronchi-Bronchioles:
A. Functions to:
1. Warm and humidify the air
2. Distribute air to the lungs
3. Defense system (remove dust and bacteria)
B. Supplied by separate circulatory system bronchial circulation-part of the systemic circulation.
C. Trachea and bronchi lined with ciliated, mucous coated epithelium that aid in clearing passageway. Cilia beat toward the pharynx.
-Epithelium rests on smooth muscle (can constrict or dilate independent of the lung) and is supported by cartilage.
D. Bronchioles: Lack cartilage, simple cuboidal epithelium, volume depends on lung volume.
-have sensory cells sensitive to stretch and irritants
**NO GAS EXCHANGE TAKES PLACE IN THE CONDUCTING ZONE-DEAD SPACE
Respiratory Zone: Alveolar duct and alveolar sacs.
A. SITE OF GAS EXCHANGE
B. Has it’s own circulation: the pulmonary circulation
-in order to match ventilation, follows and branches along with the pulmonary tree.
-pulmonary artery from right ventricle supplies nutrients to the alveolar walls
-capillary surface area nearly as great as the alveolar surface area
-can increase from 70 ml (normal) to 200 ml (exercise) recruitment
-capillaries also cover several alveoli, increase time of exposure of red blood cells to alveolar gas
C. Terminal Respiratory Unit: functional exchange unit of lungs
Greatly increases surface area: 60,000 terminal respiratory units, each with 5000 alveoli and 250 alveolar ducts.
II. VENTILATION:
Main purpose is to maintain an optimal concentration of O2 and CO2 in the alveolar gas.
How do we move air into and out of the lungs.
1. The lungs are housed in an airtight cavity, the thoracic cavity, that is separated from the abdomen by a large dome-shaped muscle, the diaphragm. Lungs conform to the thoracic cavity by contact of fluid lined pleura:
visceral pleura: covers the lungs
parietal pleura: lines the thoracic cavity
2. The anterior portion of the thoracic cavity is bounded by the ribs. The external and internal intercostal muscles lie between the ribs. The ribs are hinged on one side to the vertebral column and on the other to the sternum.
A. Inspiration:
The primary inspiratory muscle is the diaphragm. The diaphragm is a skeletal muscle and is innervated by the phrenic nerve. The diaphragm contracts during every inspiration.
-contraction of the diaphragm increases the vertical diameter of the thoracic cavity.
Voluntary muscles
The external intercostals raise the rib cage and increase the anterior-posterior diameter of the thoracic cavity.
Accessory muscles
Active during forced breathing. These include the scalene muscles of the neck. The sternocleidomastoids insert on the top of the sternum. These muscles elevate the upper rib cage during heavy breathing such as during exercise.
B. Expiration:
During normal tidal breathing at the end of inspiration the diaphragm relaxes, and expiration is a passive process. The natural recoil tendency of the lungs and chest wall cause deflation of the lungs.
-elastic fibers
-surface tension
During forced expiration other expiratory muscles become active
-internal intercostals oppose the external intercostals and pull the rib cage down.
-abdominal muscles force the contents of the abdominal cavity up against the diaphragm.
Especially important in coughing, vomiting, etc.
C. Pressures:
Airflow is due to changes in pressure in the thoracic cavity that are transmitted to the alveoli.
Three important pressures associated with breathing and airflow:
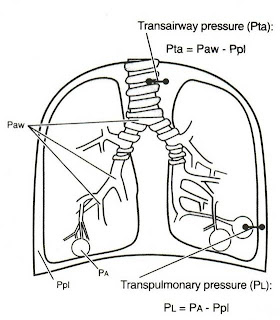
1. Pleural pressure (PPL): pressure in the pleural fluid between the lung and chest wall.
2. Alveolar pressure (PA): pressure inside the alveoli.
3. Transmural pressure (PTM): the pressure difference across the airway or across the lung wall.
-Transpulmonary pressure: alveolar pressure-pleural pressure. Keeps the lungs from collapsing. Is always positive during normal breathing.
-Transairway pressure: airway pressure-pleural pressure. Transairway pressure is important in keeping the airways open during expiration.
Pressures (cont’d)
Inspiration:
PPL is negative during quiet breathing and becomes more negative during inspiration. This causes PA to drop with respect to atmospheric pressure (very little pressure needed, -1 mmHg)
Expiration:
PPL becomes less negative and PA becomes slightly positive (+1 mmHg)
During heavy breathing PA can go from -80 to 100 mmHg
Pressures (cont’d)
Pneumothorax: hole in the thoracic cavity, PPL becomes 0, can no longer generate (-) pressures in the alveoli.
D. Compliance:
Compliance: the ease with which the lungs can be distended.
-how well the lung inflates and deflates with a change in transpulmonary pressure is a function of the elastic properties of the lung.
Compliance (cont’d)
Pressure-volume relations: elastic properties of the lungs can be determined by measuring changes in lung volume that occur with changes in pressure.
Compliance=V/P: volume increase in lungs for each unit increase in pressure
normal ~0.13L/cm (lungs alone are more compliant than this, but part of energy must go to expand the thoracic cage).
Compliance can be measured in human lungs by measuring the pleural pressure and the volume of the lungs with a spirometer.
E. Surface tension:
•Within water the forces on water molecules attract one another, at the surface, the attraction is stronger from molecules under the surface.
The surface of the alveoli are moist, creating an air-liquid interface in the alveoli, very high surface tension would make lungs very non-compliant. Compare to saline filled lung (no air-water interface) that is much more compliant.
•Surfactant: a special lipoprotein mixture coating the surface of alveoli.
•-synthesized in alveolar type II cells
-main ingredient is dipalmitoyl phosphatidylcholine (DPPC)
Functions of Surfactant:
•1. Reduces muscular effort of breathing (makes lungs more compliant).
•2. Reduces elastic recoil of the lungs at low volume (prevents alveoli from collapsing)
•3. Maintains the equality of size of alveoli during inflation/deflation
•-as alveoli become smaller decreases surface tension more, makes smaller alveoli easier to inflate. As alveoli become larger increases surface tension, harder to inflate.
•4. Responsible for difference in inflation vs deflation curve.
•-during deflation, surfactant molecules are squeezed together lowering the surface tension.
Forced Vital Capacity
The resistance to airflow can not be measured directly, but must be calculated from the pressure gradient and airflow during a breath.
One way of indirectly assessing resistance is to look at the results of a forced expiration into a spirometer:
Forced Vital Capacity (FVC): Large breath from FRC to TLC and breath out as hard and fast as possible.
III. PULMONARY VOLUMES AND CAPACITIES
•Can be measured with a spirometer.(except RV)
A. Four different volumes
1. Tidal volume (TV): volume of air inspired and expired with a normal breath (.500 ml).
2. Inspiratory Reserve Volume (IRV): extra volume of air that can be inspired after a normal tidal inspiration (.3000 ml).
3. Expiratory Reserve Volume (ERV): extra volume of air that can be expired after a normal tidal expiration (.1100 ml).
4. Residual Volume (RV): volume of air remaining after a maximal expiratory effort (.1200 ml). *Can not be removed from lungs.
B. Four different capacities relating the above volumes
1. Inspiratory Capacity (IC): TV + IRV
2. Functional Residual Capacity (FRC): ERV + RV amount of air remaining in the lungs at the end of a normal tidal expiration (lungs at rest). At FRC the chest wall and lungs are recoiling in equal and opposite directions.
3. Vital Capacity (VC): IRV + TV + ERV the maximal amount of usable lung capacity.
4. Total Lung Capacity (TLC): All of the above, maximal volume to which the lungs can be expanded.
* VC is one of most important of all clinical respiratory measurements for assessing the progress of disease. Decrease compliance=decrease VC.
-restrictive diseases (limited expansion)
-large residual volume (COPD)
IV. Alveolar Ventilation
The most important aspect of breathing is to maintain an optimal concentration of O2 and CO2 in the alveolar gas.
Minute respiratory volume: total amount of air moved each minute
TV x Rate: 12 x 500=6000 ml (6L)
TV = 7-10 ml/kgBB
Physiological dead space: Due to non-functioning alveoli. Is the ADS + non-functional alveoli.
-nearly equal in normal, but in disease PDS can be 10X greater than ADS
The major purpose of breathing is to supply O2 and to remove CO2 from cells
Four major functions to achieve this goal:
1. Pulmonary ventilation: movement of air into and out of lungs
2. Diffusion of O2 and CO2 between the alveoli and the blood
3. Transport of O2 and CO2 in the blood to and from cells
4. Control of ventilation
Once the O2 is transferred to the cells it is utilized to metabolize various food molecules involving a series of enzymatic reactions. During this process there is release of energy which is stored in the form of ATP-This process is called cellular respiration.
From the time of birth until our death we breath continuously at a rate of 12-15 breaths/min. However, breathing can change in response to alterations in blood chemistry.
Breathing and gas exchange can increase 20-fold to meet the body’s energy demands during periods of need such as exercise.
I. BASIC ANATOMY:.
The lungs are composed of 2 treelike structures:
1. Vascular tree: consists of arteries and veins connected by capillaries
2. Airway tree: consists of hollow branching tubes that conduct air from the environment to site of gas exchange to the blood.
Conducting Zone: (in descending order): Nose (conchae)-Pharynx-Larynx-Trachea-Bronchi-Bronchioles:
A. Functions to:
1. Warm and humidify the air
2. Distribute air to the lungs
3. Defense system (remove dust and bacteria)
B. Supplied by separate circulatory system bronchial circulation-part of the systemic circulation.
C. Trachea and bronchi lined with ciliated, mucous coated epithelium that aid in clearing passageway. Cilia beat toward the pharynx.
-Epithelium rests on smooth muscle (can constrict or dilate independent of the lung) and is supported by cartilage.
D. Bronchioles: Lack cartilage, simple cuboidal epithelium, volume depends on lung volume.
-have sensory cells sensitive to stretch and irritants
**NO GAS EXCHANGE TAKES PLACE IN THE CONDUCTING ZONE-DEAD SPACE
Respiratory Zone: Alveolar duct and alveolar sacs.
A. SITE OF GAS EXCHANGE
B. Has it’s own circulation: the pulmonary circulation
-in order to match ventilation, follows and branches along with the pulmonary tree.
-pulmonary artery from right ventricle supplies nutrients to the alveolar walls
-capillary surface area nearly as great as the alveolar surface area
-can increase from 70 ml (normal) to 200 ml (exercise) recruitment
-capillaries also cover several alveoli, increase time of exposure of red blood cells to alveolar gas
C. Terminal Respiratory Unit: functional exchange unit of lungs
Greatly increases surface area: 60,000 terminal respiratory units, each with 5000 alveoli and 250 alveolar ducts.
II. VENTILATION:
Main purpose is to maintain an optimal concentration of O2 and CO2 in the alveolar gas.
How do we move air into and out of the lungs.
1. The lungs are housed in an airtight cavity, the thoracic cavity, that is separated from the abdomen by a large dome-shaped muscle, the diaphragm. Lungs conform to the thoracic cavity by contact of fluid lined pleura:
visceral pleura: covers the lungs
parietal pleura: lines the thoracic cavity
2. The anterior portion of the thoracic cavity is bounded by the ribs. The external and internal intercostal muscles lie between the ribs. The ribs are hinged on one side to the vertebral column and on the other to the sternum.
A. Inspiration:
The primary inspiratory muscle is the diaphragm. The diaphragm is a skeletal muscle and is innervated by the phrenic nerve. The diaphragm contracts during every inspiration.
-contraction of the diaphragm increases the vertical diameter of the thoracic cavity.
Voluntary muscles
The external intercostals raise the rib cage and increase the anterior-posterior diameter of the thoracic cavity.
Accessory muscles
Active during forced breathing. These include the scalene muscles of the neck. The sternocleidomastoids insert on the top of the sternum. These muscles elevate the upper rib cage during heavy breathing such as during exercise.
B. Expiration:
During normal tidal breathing at the end of inspiration the diaphragm relaxes, and expiration is a passive process. The natural recoil tendency of the lungs and chest wall cause deflation of the lungs.
-elastic fibers
-surface tension
During forced expiration other expiratory muscles become active
-internal intercostals oppose the external intercostals and pull the rib cage down.
-abdominal muscles force the contents of the abdominal cavity up against the diaphragm.
Especially important in coughing, vomiting, etc.
C. Pressures:
Airflow is due to changes in pressure in the thoracic cavity that are transmitted to the alveoli.
Three important pressures associated with breathing and airflow:
1. Pleural pressure (PPL): pressure in the pleural fluid between the lung and chest wall.
2. Alveolar pressure (PA): pressure inside the alveoli.
3. Transmural pressure (PTM): the pressure difference across the airway or across the lung wall.
-Transpulmonary pressure: alveolar pressure-pleural pressure. Keeps the lungs from collapsing. Is always positive during normal breathing.
-Transairway pressure: airway pressure-pleural pressure. Transairway pressure is important in keeping the airways open during expiration.
Pressures (cont’d)
Inspiration:
PPL is negative during quiet breathing and becomes more negative during inspiration. This causes PA to drop with respect to atmospheric pressure (very little pressure needed, -1 mmHg)
Expiration:
PPL becomes less negative and PA becomes slightly positive (+1 mmHg)
During heavy breathing PA can go from -80 to 100 mmHg
Pressures (cont’d)
Pneumothorax: hole in the thoracic cavity, PPL becomes 0, can no longer generate (-) pressures in the alveoli.
D. Compliance:
Compliance: the ease with which the lungs can be distended.
-how well the lung inflates and deflates with a change in transpulmonary pressure is a function of the elastic properties of the lung.
Compliance (cont’d)
Pressure-volume relations: elastic properties of the lungs can be determined by measuring changes in lung volume that occur with changes in pressure.
Compliance=V/P: volume increase in lungs for each unit increase in pressure
normal ~0.13L/cm (lungs alone are more compliant than this, but part of energy must go to expand the thoracic cage).
Compliance can be measured in human lungs by measuring the pleural pressure and the volume of the lungs with a spirometer.
E. Surface tension:
•Within water the forces on water molecules attract one another, at the surface, the attraction is stronger from molecules under the surface.
The surface of the alveoli are moist, creating an air-liquid interface in the alveoli, very high surface tension would make lungs very non-compliant. Compare to saline filled lung (no air-water interface) that is much more compliant.
•Surfactant: a special lipoprotein mixture coating the surface of alveoli.
•-synthesized in alveolar type II cells
-main ingredient is dipalmitoyl phosphatidylcholine (DPPC)
Functions of Surfactant:
•1. Reduces muscular effort of breathing (makes lungs more compliant).
•2. Reduces elastic recoil of the lungs at low volume (prevents alveoli from collapsing)
•3. Maintains the equality of size of alveoli during inflation/deflation
•-as alveoli become smaller decreases surface tension more, makes smaller alveoli easier to inflate. As alveoli become larger increases surface tension, harder to inflate.
•4. Responsible for difference in inflation vs deflation curve.
•-during deflation, surfactant molecules are squeezed together lowering the surface tension.
Forced Vital Capacity
The resistance to airflow can not be measured directly, but must be calculated from the pressure gradient and airflow during a breath.
One way of indirectly assessing resistance is to look at the results of a forced expiration into a spirometer:
Forced Vital Capacity (FVC): Large breath from FRC to TLC and breath out as hard and fast as possible.
III. PULMONARY VOLUMES AND CAPACITIES
•Can be measured with a spirometer.(except RV)
A. Four different volumes
1. Tidal volume (TV): volume of air inspired and expired with a normal breath (.500 ml).
2. Inspiratory Reserve Volume (IRV): extra volume of air that can be inspired after a normal tidal inspiration (.3000 ml).
3. Expiratory Reserve Volume (ERV): extra volume of air that can be expired after a normal tidal expiration (.1100 ml).
4. Residual Volume (RV): volume of air remaining after a maximal expiratory effort (.1200 ml). *Can not be removed from lungs.
B. Four different capacities relating the above volumes
1. Inspiratory Capacity (IC): TV + IRV
2. Functional Residual Capacity (FRC): ERV + RV amount of air remaining in the lungs at the end of a normal tidal expiration (lungs at rest). At FRC the chest wall and lungs are recoiling in equal and opposite directions.
3. Vital Capacity (VC): IRV + TV + ERV the maximal amount of usable lung capacity.
4. Total Lung Capacity (TLC): All of the above, maximal volume to which the lungs can be expanded.
* VC is one of most important of all clinical respiratory measurements for assessing the progress of disease. Decrease compliance=decrease VC.
-restrictive diseases (limited expansion)
-large residual volume (COPD)
IV. Alveolar Ventilation
The most important aspect of breathing is to maintain an optimal concentration of O2 and CO2 in the alveolar gas.
Minute respiratory volume: total amount of air moved each minute
TV x Rate: 12 x 500=6000 ml (6L)
TV = 7-10 ml/kgBB
Physiological dead space: Due to non-functioning alveoli. Is the ADS + non-functional alveoli.
-nearly equal in normal, but in disease PDS can be 10X greater than ADS